My life with Lyme
I am not writing this because I want people to feel sorry for me. I’m doing fine now, really. I just want to warn people that this could happen to them, too.
I don’t know when the tick attached itself—probably when I was tree-planting near Babine Lake in 1989, or during a trip in the western States. I didn’t see or feel the tick when it bit me, but the bacteria it injected into my blood have severely affected my life (and my family’s) for the past 20 years.
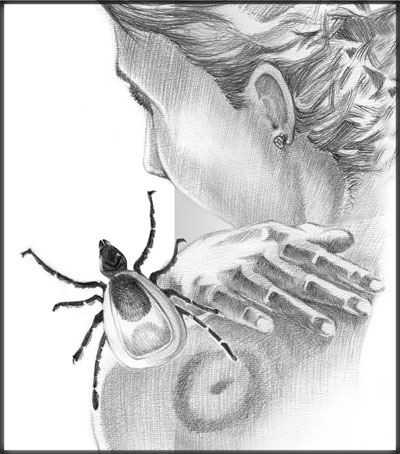
I had never heard of Lyme disease back in 1989 when I discovered what is commonly called a ‘bull’s-eye-rash’ on my leg. Starting as a raised, red, itchy circle about two centimetres wide, it came and went several times, growing until it was 12 centimetres across. I contemplated seeing a doctor, but then it disappeared and didn’t come back. I thought it had just been a spider bite, and promptly forgot about it. Big mistake!
Until then I had been a fitness nut: jogging, marathon skiing, and mountain hiking; I thought nothing of grueling treks with a heavy pack. But soon my adventures started to leave me very fatigued, and I backed off a bit. My health seemed stable though, and I became pregnant with my son two years later. I felt wonderful during the pregnancy, hiking and skiing throughout.
But when my son was born, one month prematurely, everything went downhill fast. I was exhausted all the time. Every morning I felt like I’d been hit by a truck, hurting all over: joints, muscles, sore throat, headache. But I would drag myself out of bed to deal with my newborn, thinking my fatigue was just part of being a new mom.
But as the months and years went by, things didn’t improve. I blamed it on stress: my son also had health problems, like constant diarrhea and an inability to put on weight. Desperate, I insisted the pediatrician treat my son for Giardia, or ‘Beaver Fever’ (which produces symptoms very similar to those he was suffering), using a combination of two powerful antibiotics (coincidentally, they are the same two drugs that are used to treat Lyme disease). Within two weeks he was a new boy, and started to thrive.
My own energy continued to decline. I couldn’t walk more than 100 metres before becoming exhausted. My short-term memory, concentration and ability to think were seriously compromised. I became irritable and angry at the smallest frustrations, putting a severe strain on my marriage.
The Lyme revelation
My family doctor couldn’t offer any reason for my lack of energy. After testing me for all sorts of maladies, she finally diagnosed me with Chronic Fatigue Syndrome (CFS), for lack of anything else to label it. With no actual cure, CFS usually resolves itself over time.
But as the years went by with little or no improvement, I became desperate and started to do some research on my own. One day, after eight years of struggling with fatigue and my other symptoms, I found an article on Lyme disease, with a photo of the bull’s-eye rash I’d had.
It was an ‘Ah-hah!’ moment; all of a sudden the pieces of the puzzle fell into place. I learned there was a Dr. Murakami in Hope, BC, who treated Lyme. After waiting four months to see him, he confirmed my own diagnosis, and prescribed a combination of the same two antibiotics my son had been on—but for a whole year instead of a few weeks. It seems Lyme disease may be cured if treatment is begun immediately after the tick bite, but becomes progressively more difficult the longer it remains undiagnosed and untreated. By that time I had had the bacteria in me for 10 years! (Still, according to Dr. Murakami, I am one of the ‘lucky ones’ because I actually had a bull’s-eye rash; many people bitten by a Lyme-infected tick never get this tell-tale sign, so have no evidence of the source of their illness.)
Lyme bacteria are of the spirochete variety, like a little corkscrew, and can wriggle its way through most of our bodily membranes, allowing it to infect all systems of the body, including the brain and spinal cord. In this respect it is similar to the bacteria that causes Syphilis, which is easy to cure with antibiotics if caught early; but if not, causes permanent brain damage and other serious problems.
As my year of antibiotic treatment went by, I gradually got my energy back and was able to resume an almost normal life. I still had to be careful, though, and I was certainly not the old ‘fit-freak’ I was before; if I pushed a bit too hard, the symptoms returned.
Finding a new life
But I was having trouble coping with my office administrator job. With a poor memory and increasing dyslexia, I was always making mistakes, couldn’t remember names or dates, and misfiled or lost things. And my husband’s health was deteriorating due to stress both at work and at home.
In 2002 we drove to Alberta, looking for a new life. We discovered Lethbridge, a city we both liked, and both found work. I was doing fine—until my marriage ended (in large part, I’m sure, because of my illness and its accompanying depression). From there it was all downhill, with the stress of the illness adding to the marriage break-up, and the break-up stress compromising my immune system, allowing the disease to gain ground again.
I once again fell apart. Not able to trust my memory, and having become even more dyslexic, I knew I had to find a different way to make a living—one that didn’t involve multi-tasking, which had become almost impossible.
I came up with the idea of starting my own housekeeping company—good pay, low stress, no need for a sharp memory. But housekeeping is very physical work, and my energy levels were a major problem. I would work for two or three hours, then come home exhausted and sleep. And I needed to be in bed by eight pm each night or I couldn’t function the next day.
I developed inflammation in my muscles and joints. Because of fatigue, I had no social life. Sleep was becoming elusive—I could sleep only two hours at a time. I broke down and got a prescription for sleeping pills. My doctor was obviously very skeptical when I suggested that I might still be dealing with Lyme disease. Instead, because of my depression, she referred me to a psychiatrist who put me on anti-depressants. These lifted my mood but did nothing for my fatigue, aches and pains.
I heard of a doctor in Calgary who specialized in CFS, and got myself on her three-year waiting list. I waited, limping along, gradually getting worse. I developed fibromyalgia, suicidal depression, vision problems, and arthritis in most of my large joints. I was a mess, and in constant pain. Because of my deteriorating condition I was moved up the specialist’s waiting list, and 18 months later I finally got in to see her. I was devastated, though, when a $500 Lyme-disease lab test came back ‘inconclusive.’ I knew this meant she wouldn’t be able to do anything; the Canadian medical system won’t allow even short-term treatment of Lyme with antibiotics without a positive laboratory result. I was once again on my own.
Agonizing decision
After struggling to clean houses for three years, I finally decided I couldn’t keep it up; the work was destroying me. Even with medication I was severely depressed. I had inflamed joints and arthritis in my hips, neck, back and shoulders—and I was totally, utterly, exhausted. I applied for Assisted Income for the Severely Handicapped. After waiting for months I was told I was not eligible.
At that point I had to accept that I couldn’t afford to support myself and my then 16-year-old son, and made the agonizing decision to return to Smithers on my own, leaving my son behind in Lethbridge in his father’s care. I planned to stay with my parents until things somehow turned around.
Back in Smithers, the doctor I saw dropped me like a hot potato when I said I thought I had Lyme. He quickly referred me to a contagious-disease specialist from Nanaimo.
When I saw this specialist months later, he said, “There is no possible way you could have had Lyme disease for so long and still be alive!” (This, however, is contrary to my research: tens of thousands of people with Lyme in the USA alone survive year after year, albeit debilitated with fatigue and other symptoms.) He thought I almost surely had a rare case of CFS.
At the moment, there is still no accurate test for Lyme disease, and little research to develop one. With no reliable test, how do you determine whether to begin expensive, long-term treatment? There is much controversy as to how to treat chronic Lyme, with two warring camps within the medical profession and government officials.
On one side are those who believe long-term antibiotics are the only way to cure this devastating illness. Dr. Murakami is of this camp, and has successfully treated many chronic Lyme patients with long-term antibiotics. But he has been challenged by the College of Physicians and Surgeons, with warnings that he could lose his license if he continues his treatment methods. This has sent a strong message to all physicians in Canada: DO NOT treat chronic Lyme with long-term antibiotics: we can’t afford it. Murakami’s case was helped by lobbying from his cured patients.
On the other side are those who oppose long-term antibiotics, and refuse to prescribe them. This camp includes the Canadian government and the medical establishment, who refuse to acknowledge that Lyme disease is a problem in Canada, even though, just across the border, thousands of people have been diagnosed clinically and successfully treated. Apparently, this head-in-the-sand attitude comes from the Canadian government’s awareness that there are probably thousands of improperly diagnosed, untreated, chronic Lyme patients in Canada, currently diagnosed with untreatable CFS, fibromyalgia or lupus, who would need expensive, long-term intravenous medication if formally diagnosed with Lyme. (Recently, the US government put a cap on the length of anti-biotic treatment allowed for Lyme, due to lobbying by medical insurance companies that are having to pay out more and more for long-term treatment of Lyme patients.)
Meanwhile, I live with the fear that my son will get full-blown Lyme disease: the bacterium is very pervasive and persistent. It can lie dormant in the nervous system (brain, spinal cord, and nerves) for years…until the immune system is compromised by another illness or stress, and then reactivates and multiplies. It easily passes across the placental barrier, and my son was inside me after I had the bull’s-eye rash. He shares many of my symptoms, but right now his immune system is strong and healthy. I worry what will happen if he gets run down (a bad case of flu, for example, or a traumatic event) and his immune system becomes overwhelmed, as mine did. But there is nothing I can do but wait, watch, and hope for the best. Researchers are discovering that genetics plays a large role in how sick people get with Lyme: some have few symptoms, while others are killed by it. I live with the hope that he has the right genes.
I believe that those in power have estimated that the very high cost of treating all these patients will bring an already under-funded, over-burdened medical system to its knees. There is also a lot of money being pumped into the Canadian economy as all these patients, left to their own devices, try to cure their illnesses and alleviate their symptoms with over-the-counter medications and supplements.
I have re-applied for a Canada Disability Pension, and wait (once more) to hear the verdict, relying on my parents’ undying support, and resting. It has been a long, difficult 20 years, with little or no help from the ‘professionals,’ who seem to be intent on continuing a long-term debate regarding the actual existence and/or proper treatment of the disease.
There is a standing joke among Lyme sufferers: One ‘Lymer’ says to another, “Oh well, at least it isn’t fatal.” The other replies, “No, we just wish it was!”
So, if you go out into the woods, please cover up: long pants, long-sleeve shirt, socks and shoes or boots. And check yourself over at the end of the day…they’re here, waiting for you to pick them up!